

CN 11-4766/R
主办:中国科学院心理研究所
出版:科学出版社


心理科学进展 ›› 2026, Vol. 34 ›› Issue (1): 108-122.doi: 10.3724/SP.J.1042.2026.0108 cstr: 32111.14.2026.0108
收稿日期:2025-04-24
出版日期:2026-01-15
发布日期:2025-11-10
通讯作者:
张丹丹, E-mail: zhangdd05@gmail.com基金资助:
GAO Kexiang, TANG Yuyao, ZHANG Yueyao, ZHANG Dandan( )
)
Received:2025-04-24
Online:2026-01-15
Published:2025-11-10
摘要:
内隐情绪调节是个体在无意识监督或不具有明确的情绪调节意图下改变情绪的过程。与外显情绪调节相比, 内隐情绪调节对前额叶执行控制系统的依赖度更低。本文在已有的内隐情绪调节二分类基础上, 提出了新的三分类理论框架, 将内隐情绪调节分为:自动化、任务附加型、内隐目标驱动三个内隐情绪调节种类。其中, 自动化内隐调节以恐惧消退为代表, 依赖腹内侧前额叶直接调控杏仁核; 任务附加型调节发生在情绪标签、情绪Stroop等任务中, 外侧前额叶通过认知控制系统, 在任务执行过程中附带地调节情绪; 内隐目标驱动型调节则通过启动或内隐训练, 激活内隐情绪调节目标追求, 既可借助腹内侧前额叶实现自动化调节, 又可在一定条件下调用外侧前额叶的认知控制功能实现受控情绪调节。神经调控研究证实, 腹内侧前额叶是内隐情绪调节的关键性因果脑区, 其功能增强有望改善抑郁和焦虑患者的内隐情绪调节能力。本文提出的三分类理论框架突出了内隐情绪调节的多样化机制, 拓展了情绪调节理论的动态性理解, 同时也为情绪障碍患者的临床干预提供了有潜力的新途径。
中图分类号:
高可翔, 汤煜尧, 张岳瑶, 张丹丹. (2026). 内隐情绪调节的认知神经机制. 心理科学进展 , 34(1), 108-122.
GAO Kexiang, TANG Yuyao, ZHANG Yueyao, ZHANG Dandan. (2026). The cognitive and neural mechanisms of implicit emotion regulation. Advances in Psychological Science, 34(1), 108-122.
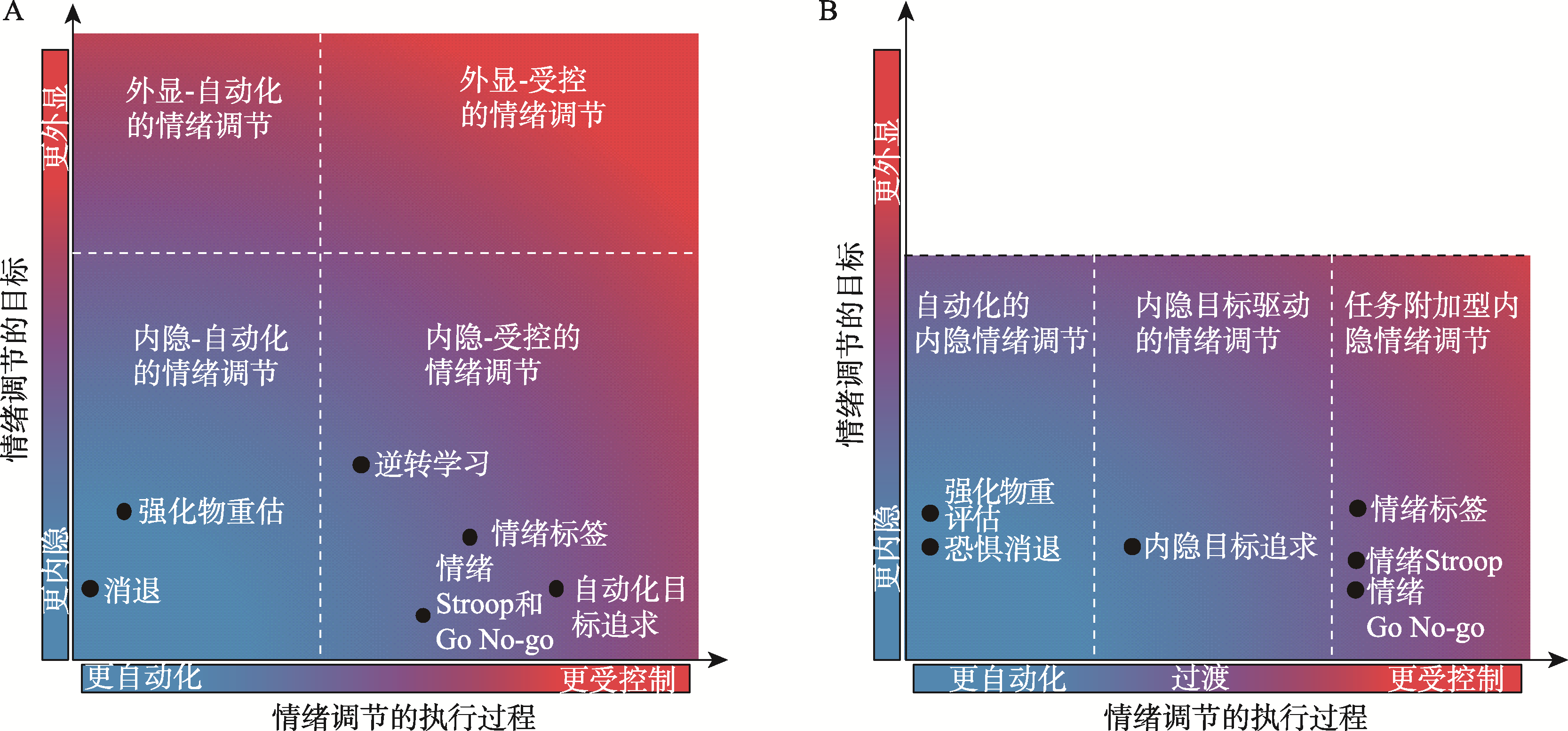
图1 内隐情绪调节的分类。A.本图改编自情绪调节领域著名学者Gross提出的情绪调节多维框架, 它将内隐情绪调节分为“内隐自动化的情绪调节”和“内隐受控的情绪调节”两类(Braunstein et al., 2017)。B.本文提出的内隐情绪调节三分类框架, 包括“自动化的内隐情绪调节”, “任务附加型内隐情绪调节”和“内隐目标驱动的情绪调节”三类。
| [1] |
高可翔, 张岳瑶, 李思瑾, 袁加锦, 李红, 张丹丹. (2023). 腹内侧前额叶在内隐认知重评中的因果作用. 心理学报, 55(2), 210-223.
doi: 10.3724/SP.J.1041.2023.00210 |
| [2] |
华艳, 李明霞, 王巧婷, 冯彩霞, 张晶. (2020). 左侧眶额皮层在自动情绪调节下注意选择中的作用:来自经颅直流电刺激的证据. 心理学报, 52(9), 1048-1056.
doi: 10.3724/SP.J.1041.2020.01048 |
| [3] |
莫李澄, 郭田友, 张岳瑶, 徐锋, 张丹丹. (2021). 激活右腹外侧前额叶提高抑郁症患者对社会疼痛的情绪调节能力:一项TMS研究. 心理学报, 53(5), 494-504
doi: 10.3724/SP.J.1041.2021.00494 |
| [4] | 莫李澄, 李思瑾, 张丹丹. (2024b). 社会疼痛情绪调节的神经机制. 心理科学, 47(3), 530-537. |
| [5] | 莫李澄, 李宜伟, 张丹丹. (2024a). 社会疼痛情绪调节的认知神经机制: 现状及展望. 应用心理学, 30(1), 33-43. |
| [6] | 张丹丹, 李思瑾. (2024). 情绪调节的神经环路及其在情绪障碍人群中的表现. 四川师范大学学报(自然科学版), 47(3), 285-293. |
| [7] |
Abend R., Sar-el R., Gonen T., Jalon I., Vaisvaser S., Bar-Haim Y., & Hendler T. (2019). Modulating emotional experience using electrical stimulation of the medial- prefrontal cortex: A preliminary tDCS-fMRI study. Neuromodulation, 22(8), 884-893. https://doi.org/10.1111/ner.12787
doi: 10.1111/ner.12787 URL pmid: 29741803 |
| [8] |
Aldao A., Nolen-Hoeksema S., & Schweizer S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217-237. https://doi.org/10.1016/j.cpr.2009.11.004
doi: 10.1016/j.cpr.2009.11.004 URL pmid: 20015584 |
| [9] |
Bermpohl F., Fregni F., Boggio P. S., Thut G., Northoff G., Otachi P. T., … Pascual-Leone A. (2005). Left prefrontal repetitive transcranial magnetic stimulation impairs performance in affective go/no-go task. Neuroreport, 16(6), 615-619. https://doi.org/10.1097/00001756-200504250-00020
URL pmid: 15812319 |
| [10] |
Bermpohl F., Fregni F., Boggio P. S., Thut G., Northoff G., Otachi P. T. M., … Pascual-Leone A. (2006). Effect of low-frequency transcranial magnetic stimulation on an affective go/no-go task in patients with major depression: Role of stimulation site and depression severity. Psychiatry Research, 141(1), 1-13. https://doi.org/10.1016/j.psychres.2005.07.018
URL pmid: 16352348 |
| [11] |
Bouton M. E. (2024). Habit and persistence. Journal of the Experimental Analysis of Behavior, 121(1), 88-96. https://doi.org/10.1002/jeab.894
doi: 10.1002/jeab.894 URL pmid: 38149526 |
| [12] |
Brandl F., Weise B., Mulej Bratec S., Jassim N., Hoffmann Ayala D., Bertram T., Ploner M., & Sorg C. (2022). Common and specific large-scale brain changes in major depressive disorder, anxiety disorders, and chronic pain: A transdiagnostic multimodal meta-analysis of structural and functional MRI studies. Neuropsychopharmacology, 47(5), 1071-1080. https://doi.org/10.1038/s41386-022-01271-y
doi: 10.1038/s41386-022-01271-y URL pmid: 35058584 |
| [13] |
Brändle F., Wu C. M., & Schulz E. (2020). What are we curious about? Trends in Cognitive Sciences, 24(9), 685-687. https://doi.org/10.1016/j.tics.2020.05.010
doi: S1364-6613(20)30134-0 URL pmid: 32622725 |
| [14] |
Braunstein L. M., Gross J. J., & Ochsner K. N. (2017). Explicit and implicit emotion regulation: A multi-level framework. Social Cognitive and Affective Neuroscience, 12(10), 1545-1557. https://doi.org/10.1093/scan/nsx096
doi: 10.1093/scan/nsx096 URL pmid: 28981910 |
| [15] | Brown E. C., Artigas S. O., Elsner S., Liu L., & Park S. Q. (2025). Utilizing rewards to dampen fear and its recovery. Scientific Reports, 15(1), 17671. https://doi.org/10.1038/s41598-025-99758-3 |
| [16] | Bukalo O., Pinard C. R., Silverstein S., Brehm C., Hartley N. D., Whittle N., … Holmes A. (2015). Prefrontal inputs to the amygdala instruct fear extinction memory formation. Science Advances, 1(6), e1500251. https://doi.org/10.1126/sciadv.1500251 |
| [17] |
Burklund L. J., Craske M. G., Taylor S. E., & Lieberman M. D. (2015). Altered emotion regulation capacity in social phobia as a function of comorbidity. Social Cognitive and Affective Neuroscience, 10(2), 199-208. https://doi.org/10.1093/scan/nsu058
doi: 10.1093/scan/nsu058 URL pmid: 24813437 |
| [18] |
Calhoon G. G., & Tye K. M. (2015). Resolving the neural circuits of anxiety. Nature Neuroscience, 18(10), 1394-1404. https://doi.org/10.1038/nn.4101
doi: 10.1038/nn.4101 URL pmid: 26404714 |
| [19] | Cao D., Li Y., Niznikiewicz M. A., Tang Y., & Wang J. (2018). The theta burst transcranial magnetic stimulation over the right PFC affects electroencephalogram oscillation during emotional processing. Progress in Neuro- Psychopharmacology and Biological Psychiatry, 82, 21-30. https://doi.org/10.1016/j.pnpbp.2017.12.005 |
| [20] | Cohen, J. R., & Lieberman M. D. (2010). The common neural basis of exerting self-control in multiple domains. In R. Hassin etal. (Eds.) Self control in society, mind, and brain (pp. 141-162). Oxford Academic. https://doi.org/10.1093/acprof:oso/9780195391381.003.0008 |
| [21] | Cremers H., Keedy S., & Coccaro E. (2021). The development of an fMRI protocol to investigate vmPFC network functioning underlying the generalization of behavioral control. Psychiatry Research: Neuroimaging, 307, 111197. https://doi.org/10.1016/j.pscychresns.2020.111197 |
| [22] |
Custers R., & Aarts H. (2010). The unconscious will: How the pursuit of goals operates outside of conscious awareness. Science, 329(5987), 47-50. https://doi.org/10.1126/science.1188595
doi: 10.1126/science.1188595 URL pmid: 20595607 |
| [23] |
Dalton S. D. P., Cooper H., Jennings B., & Cheeta S. (2025). The empirical status of implicit emotion regulation in mood and anxiety disorders: A meta-analytic review. Journal of Affective Disorders, 380, 256-269. Advance online publication. https://doi.org/10.1016/j.jad.2025.03.118
doi: 10.1016/j.jad.2025.03.118 URL pmid: 40122263 |
| [24] | Diekhof E. K., Geier K., Falkai P., & Gruber O. (2011). Fear is only as deep as the mind allows: A coordinate- based meta-analysis of neuroimaging studies on the regulation of negative affect. NeuroImage, 58(1), 275-285. https://doi.org/10.1016/j.neuroimage.2011.05.073 |
| [25] |
Dixon M. L., Thiruchselvam R., Todd R., & Christoff K. (2017). Emotion and the prefrontal cortex: An integrative review. Psychological Bulletin, 143(10), 1033-1081. https://doi.org/10.1037/bul0000096
doi: 10.1037/bul0000096 URL pmid: 28616997 |
| [26] |
Drakaki M., Mathiesen C., Siebner H. R., Madsen K., & Thielscher A. (2022). Database of 25 validated coil models for electric field simulations for TMS. Brain Stimulation, 15(3), 697-706. https://doi.org/10.1016/j.brs.2022.04.017
doi: 10.1016/j.brs.2022.04.017 URL pmid: 35490970 |
| [27] |
Dunsmoor J. E., Niv Y., Daw N., & Phelps E. A. (2015). Rethinking extinction. Neuron, 88(1), 47-63. https://doi.org/10.1016/j.neuron.2015.09.028
doi: 10.1016/j.neuron.2015.09.028 URL pmid: 26447572 |
| [28] | Elwood L. S., Wolitzky-Taylor K., & Olatunji B. O. (2012). Measurement of anxious traits: A contemporary review and synthesis. Anxiety, Stress and Coping, 25(6), 647-666. https://doi.org/10.1080/10615806.2011.582949 |
| [29] |
Etkin A., Büchel C., & Gross J. J. (2015). The neural bases of emotion regulation. Nature Reviews Neuroscience, 16(11), 693-700. https://doi.org/10.1038/nrn4044
doi: 10.1038/nrn4044 URL pmid: 26481098 |
| [30] | Ferri J., Schmidt J., Hajcak G., & Canli T. (2016). Emotion regulation and amygdala-precuneus connectivity: Focusing on attentional deployment. Cognitive, Affective & Behavioral Neuroscience, 16(6), 991-1002. https://doi.org/10.3758/s13415-016-0447-y |
| [31] |
Gallo I. S., & Gollwitzer P. M. (2007). Implementation intentions: Control of fear despite cognitive load. Psicothema, 19(2), 280-285.
pmid: 17425900 |
| [32] |
Gallo I. S., Keil A., McCulloch K. C., Rockstroh B., & Gollwitzer P. M. (2009). Strategic automation of emotion regulation. Journal of Personality and Social Psychology, 96(1), 11-31. https://doi.org/10.1037/a0013460
doi: 10.1037/a0013460 URL pmid: 19210061 |
| [33] | Gao K., Wong A. B., Li S., Zhang Y., & Zhang D. (2024). The ventromedial prefrontal cortex plays an important role in implicit emotion regulation: A focality-optimized multichannel tDCS study in anxiety individuals. Human Brain Mapping, 45(13), e26812. https://doi.org/10.1002/hbm.26812 |
| [34] | Gao W., Yan X., & Yuan J. (2022). Neural correlations between cognitive deficits and emotion regulation strategies: understanding emotion dysregulation in depression from the perspective of cognitive control and cognitive biases. Psychoradiology, 2(3), 86-99. https://doi.org/10.1093/psyrad/kkac014 |
| [35] |
Gilam G., Abend R., Gurevitch G., Erdman A., Baker H., Ben-Zion Z., & Hendler T. (2018). Attenuating anger and aggression with neuromodulation of the vmPFC: A simultaneous tDCS-fMRI study. Cortex, 109, 156-170. https://doi.org/10.1016/j.cortex.2018.09.010
doi: S0010-9452(18)30309-5 URL pmid: 30343211 |
| [36] |
Goode T. D., & Maren S. (2019). Common neurocircuitry mediating drug and fear relapse in preclinical models. Psychopharmacology, 236(1), 415-437. https://doi.org/10.1007/s00213-018-5024-3
doi: 10.1007/s00213-018-5024-3 URL pmid: 30255379 |
| [37] |
Gottfried J. A., & Dolan R. J. (2004). Human orbitofrontal cortex mediates extinction learning while accessing conditioned representations of value. Nature Neuroscience, 7(10), 1144-1152. https://doi.org/10.1038/nn1314
URL pmid: 15361879 |
| [38] | Gross J. J. (2015). The extended process model of emotion regulation: Elaborations, applications, and future directions. Psychological Inquiry, 26(1), 130-137. https://doi.org/10.1080/1047840X.2015.989751 |
| [39] | Gross J. J., & Jazaieri H. (2014). Emotion, emotion regulation, and psychopathology: An affective science perspective. Clinical Psychological Science, 2(4), 387-401. https://doi.org/10.1177/2167702614536164 |
| [40] |
Gross J. J., & John O. P. (2003). Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology, 85(2), 348-362. https://doi.org/10.1037/0022-3514.85.2.348
doi: 10.1037/0022-3514.85.2.348 URL pmid: 12916575 |
| [41] | Gyurak A., Gross J. J., & Etkin A. (2011). Explicit and implicit emotion regulation: A dual-process framework. Cognition and Emotion, 25(3), 400-412. https://doi.org/10.1080/02699931003782614 |
| [42] |
He Z., Li S., Mo L., Zheng Z., Li Y., Li H., & Zhang D. (2023). The VLPFC-engaged voluntary emotion regulation: Combined TMS-fMRI evidence for the neural circuit of cognitive reappraisal. Journal of Neuroscience, 43(34), 6046-6060. https://doi.org/10.1523/JNEUROSCI.1337-22.2023
doi: 10.1523/JNEUROSCI.1337-22.2023 URL pmid: 37507228 |
| [43] |
Heller A. S., Johnstone T., Shackman A. J., Light S. N., Peterson M. J., Kolden G. G., Kalin N. H., & Davidson R. J. (2009). Reduced capacity to sustain positive emotion in major depression reflects diminished maintenance of fronto-striatal brain activation. Proceedings of the National Academy of Sciences of the United States of America, 106(52), 22445-22450. https://doi.org/10.1073/pnas.0910651106
doi: 10.1073/pnas.0910651106 URL pmid: 20080793 |
| [44] |
Herrmann M. J., Katzorke A., Busch Y., Gromer D., Polak T., Pauli P., & Deckert J. (2017). Medial prefrontal cortex stimulation accelerates therapy response of exposure therapy in acrophobia. Brain Stimulation, 10(2), 291-297. https://doi.org/10.1016/j.brs.2016.11.007
doi: S1935-861X(16)30308-4 URL pmid: 27931887 |
| [45] |
Hikosaka O., & Isoda M. (2010). Switching from automatic to controlled behavior: Cortico-basal ganglia mechanisms. Trends in Cognitive Sciences, 14(4), 154-161. https://doi.org/10.1016/j.tics.2010.01.006
doi: 10.1016/j.tics.2010.01.006 URL pmid: 20181509 |
| [46] |
Hiser J., & Koenigs M. (2018). The multifaceted role of the ventromedial prefrontal cortex in emotion, decision making, social cognition, and psychopathology. Biological Psychiatry, 83(8), 638-647. https://doi.org/10.1016/j.biopsych.2017.10.030
doi: S0006-3223(17)32203-5 URL pmid: 29275839 |
| [47] | Hopp H., Troy A. S., & Mauss I. B. (2011). The unconscious pursuit of emotion regulation: Implications for psychological health. Cognition and Emotion, 25(3), 532-545. https://doi.org/10.1080/02699931.2010.532606 |
| [48] |
Ironside M., Browning M., Ansari T. L., Harvey C. J., Sekyi-Djan M. N., Bishop S. J., Harmer C. J., & O’Shea J. (2019). Effect of prefrontal cortex stimulation on regulation of amygdala response to threat in individuals with trait anxiety: A randomized clinical trial. JAMA Psychiatry, 76(1), 71-78. https://doi.org/10.1001/jamapsychiatry.2018.2172
doi: 10.1001/jamapsychiatry.2018.2172 URL pmid: 30347011 |
| [49] |
Joormann J., & Quinn M. E. (2014). Cognitive processes and emotion regulation in depression. Depression and Anxiety, 31(4), 308-315. https://doi.org/10.1002/da.22264
doi: 10.1002/da.22264 URL pmid: 24668779 |
| [50] |
Joormann J., & Stanton C. H. (2016). Examining emotion regulation in depression: A review and future directions. Behaviour Research and Therapy, 86, 35-49. https://doi.org/10.1016/j.brat.2016.07.007
doi: S0005-7967(16)30118-8 URL pmid: 27492851 |
| [51] |
Kalisch R., Korenfeld E., Stephan K. E., Weiskopf N., Seymour B., & Dolan R. J. (2006). Context-dependent human extinction memory is mediated by a ventromedial prefrontal and hippocampal network. Journal of Neuroscience, 26(37), 9503-9511. https://doi.org/10.1523/JNEUROSCI.2021-06.2006
doi: 10.1523/JNEUROSCI.2021-06.2006 URL pmid: 16971534 |
| [52] | Kenwood M. M., Kalin N. H., & Barbas H. (2022). The prefrontal cortex, pathological anxiety, and anxiety disorders. Neuropsychopharmacology, 47(1), 260-275. https://doi.org/10.1038/s41386-021-01109-z |
| [53] |
Kerns J. G., Cohen J. D., MacDonald III A. W., Cho R. Y., Stenger V. A., & Carter C. S. (2004). Anterior cingulate conflict monitoring and adjustments in control. Science, 303(5660), 1023-1026. https://doi.org/10.1126/science.1089910
doi: 10.1126/science.1089910 URL pmid: 14963333 |
| [54] | Konrad A. C., Miu A. C., Trautmann S., & Kanske P. (2025). Neural correlates and plasticity of explicit emotion regulation following the experience of trauma. Frontiers in Behavioral Neuroscience, 19, 1523035. https://doi.org/10.3389/fnbeh.2025.1523035 |
| [55] | Koole S. L., & Rothermund K. (2011). “I feel better but I don’t know why”: The psychology of implicit emotion regulation. Cognition and Emotion, 25(3), 389-399. https://doi.org/10.1080/02699931.2010.550505 |
| [56] | Koole S. L., Webb T. L., & Sheeran P. L. (2015). Implicit emotion regulation: Feeling better without knowing why. Current Opinion in Psychology, 3, 6-10. https://doi.org/10.1016/j.copsyc.2014.12.027 |
| [57] | Lapate R. C., Heckner M. K., Phan A. T., Tambini A., & D’Esposito M. (2024). Information-based TMS to mid-lateral prefrontal cortex disrupts action goals during emotional processing. Nature Communications, 15(1), 4294. https://doi.org/10.1038/s41467-024-48015-8 |
| [58] |
Lei L., Lai C. S., Lee T. M., & Lam C. L. (2024). The effect of transcranial direct current and magnetic stimulation on fear extinction and return of fear: A meta-analysis and systematic review. Journal of Affective Disorders, 362, 263-286. https://doi.org/10.1016/j.jad.2024.06.060
doi: 10.1016/j.jad.2024.06.060 URL pmid: 38908557 |
| [59] |
Li J., Schiller D., Schoenbaum G., Phelps E. A., & Daw N. D. (2011). Differential roles of human striatum and amygdala in associative learning. Nature Neuroscience, 14(10), 1250-1252. https://doi.org/10.1038/nn.2904
doi: 10.1038/nn.2904 URL pmid: 21909088 |
| [60] | Li S., Cao X., Li Y., Tang Y., Cheng S., & Zhang D. (2024). Enhancing ventrolateral prefrontal cortex activation mitigates social pain and modifies subsequent social attitudes: Insights from TMS and fMRI. NeuroImage, 292, 120620. https://doi.org/10.1016/j.neuroimage.2024.120620 |
| [61] | Li S., Chen J., Gao K., Xu F., & Zhang D. (2023). Excitatory brain stimulation over the left dorsolateral prefrontal cortex enhances voluntary distraction in depressed patients. Psychological Medicine, 53(14), 6646-6655. https://doi.org/10.1017/S0033291723000028 |
| [62] | Li Y., Li S., Li H., Tang Y., & Zhang D. (2025). fNIRS neurofeedback facilitates emotion regulation: Exploring individual differences over the ventrolateral prefrontal cortex. NeuroImage, 308, 121079. https://doi.org/10.1016/j.neuroimage.2025.121079 |
| [63] |
Lieberman M. D., Eisenberger N. I., Crockett M. J., Tom S. M., Pfeifer J. H., & Way B. M. (2007). Putting feelings into words. Psychological Science, 18(5), 421-428. https://doi.org/10.1111/j.1467-9280.2007.01916.x
URL pmid: 17576282 |
| [64] | Lincoln T. M., Schulze L., & Renneberg B. (2022). The role of emotion regulation in the characterization, development and treatment of psychopathology. Nature Reviews Psychology, 1(5), 272-286. https://doi.org/10.1038/s44159-022-00040-4 |
| [65] | Liu B., Wang Y., & Li X. (2018). Implicit emotion regulation deficits in trait anxiety: An ERP study. Frontiers in Human Neuroscience, 12, 382. https://doi.org/10.3389/fnhum.2018.00382 |
| [66] | Liu D. Y., & Thompson R. J. (2017). Selection and implementation of emotion regulation strategies in major depressive disorder: An integrative review. Clinical Psychology Review, 57(10), 183-194. https://doi.org/10.1016/j.cpr.2017.07.004 |
| [67] |
Lonsdorf T. B., Haaker J., & Kalisch R. (2014). Long-term expression of human contextual fear and extinction memories involves amygdala, hippocampus and ventromedial prefrontal cortex: A reinstatement study in two independent samples. Social Cognitive and Affective Neuroscience, 9(12), 1973-1983. https://doi.org/10.1093/scan/nsu018
doi: 10.1093/scan/nsu018 URL pmid: 24493848 |
| [68] |
Lopez-Persem A., Verhagen L., Amiez C., Petrides M., & Sallet J. (2019). The human ventromedial prefrontal cortex: Sulcal morphology and its influence on functional organization. Journal of Neuroscience, 39(19), 3627-3639. https://doi.org/10.1523/JNEUROSCI.2060-18.2019
doi: 10.1523/JNEUROSCI.2060-18.2019 URL pmid: 30833514 |
| [69] |
Lynch C. J., Elbau I. G., Ng T. H., Wolk D., Zhu S., Ayaz A., … Liston C. (2022). Automated optimization of TMS coil placement for personalized functional network engagement. Neuron, 110(20), 3263-3277.e4. https://doi.org/10.1016/j.neuron.2022.08.012
doi: 10.1016/j.neuron.2022.08.012 URL pmid: 36113473 |
| [70] |
Mackey S., & Petrides M. (2014). Architecture and morphology of the human ventromedial prefrontal cortex. European Journal of Neuroscience, 40(5), 2777-2796. https://doi.org/10.1111/ejn.12654
doi: 10.1111/ejn.12654 URL pmid: 25123211 |
| [71] |
Maren S., & Holmes A. (2016). Stress and fear extinction. Neuropsychopharmacology, 41(1), 58-79. https://doi.org/10.1038/npp.2015.180
doi: 10.1038/npp.2015.180 URL pmid: 26105142 |
| [72] | Marković V., Vicario C. M., Yavari F., Salehinejad M. A., & Nitsche M. A. (2021). A systematic review on the effect of transcranial direct current and magnetic stimulation on fear memory and extinction. Frontiers in Human Neuroscience, 15, 655947. https://doi.org/10.3389/fnhum.2021.655947 |
| [73] | Mauss I. B., Bunge S. A., & Gross J. J. (2007a). Automatic emotion regulation. Social and Personality Psychology Compass, 1(1), 146-167. https://doi.org/10.1111/j.1751-9004.2007.00005.x |
| [74] | Mauss I. B., Cook C. L., & Gross J. J. (2007b). Automatic emotion regulation during anger provocation. Journal of Experimental Social Psychology, 43(5), 698-711. https://doi.org/10.1016/j.jesp.2006.07.003 |
| [75] |
Morrison S. E., & Salzman C. D. (2010). Re-valuing the amygdala. Current Opinion in Neurobiology, 20(2), 221-230. https://doi.org/10.1016/j.conb.2010.02.007
doi: 10.1016/j.conb.2010.02.007 URL pmid: 20299204 |
| [76] |
Motzkin J. C., Philippi C. L., Wolf R. C., Baskaya M. K., & Koenigs M. (2015). Ventromedial prefrontal cortex is critical for the regulation of amygdala activity in humans. Biological Psychiatry, 77(3), 276-284. https://doi.org/10.1016/j.biopsych.2014.02.014
doi: S0006-3223(14)00109-7 URL pmid: 24673881 |
| [77] |
Oathes D. J., Zimmerman J. P., Duprat R., Japp S. S., Scully M., Rosenberg B. M., … Linn K. A. (2021). Resting fMRI-guided TMS results in subcortical and brain network modulation indexed by interleaved TMS/fMRI. Experimental Brain Research, 239(4), 1165-1178. https://doi.org/10.1007/s00221-021-06036-5
doi: 10.1007/s00221-021-06036-5 URL pmid: 33560448 |
| [78] |
Ochsner K. N., & Gross J. J. (2005). The cognitive control of emotion. Trends in Cognitive Sciences, 9(5), 242-249. https://doi.org/10.1016/j.tics.2005.03.010
doi: 10.1016/j.tics.2005.03.010 URL pmid: 15866151 |
| [79] | Ochsner K. N., Silvers J. A., & Buhle J. T. (2012). Functional imaging studies of emotion regulation:A synthetic review and evolving model of the cognitive control of emotion. Annals of the New York Academy of Sciences, 1251(1), E1-E24. https://doi.org/10.1111/j.1749-6632.2012.06751.x |
| [80] | Oyarzún J. P., Càmara E., Kouider S., Fuentemilla L., & de Diego-Balaguer R. (2019). Implicit but not explicit extinction to threat-conditioned stimulus prevents spontaneous recovery of threat-potentiated startle responses in humans. Brain and Behavior, 9(1), e01157. https://doi.org/10.1002/brb3.1157 |
| [81] | Park C., Rosenblat J. D., Lee Y., Pan Z., Cao B., Iacobucci M., & Mcintyre R. S. (2019). The neural systems of emotion regulation and abnormalities in major depressive disorder. Behavioural Brain Research, 367(4), 181-188. https://doi.org/10.1016/j.bbr.2019.04.002 |
| [82] |
Payer D. E., Baicy K., Lieberman M. D., & London E. D. (2012). Overlapping neural substrates between intentional and incidental down-regulation of negative emotions. Emotion, 12(2), 229-235. https://doi.org/10.1037/a0027421
doi: 10.1037/a0027421 URL pmid: 22468617 |
| [83] |
Phelps E. A., Delgado M. R., Nearing K. I., & LeDoux J. E. (2004). Extinction learning in humans: Role of the amygdala and vmPFC. Neuron, 43(6), 897-905. https://doi.org/10.1016/j.neuron.2004.08.042
doi: 10.1016/j.neuron.2004.08.042 URL pmid: 15363399 |
| [84] | Phillips M. L., Ladouceur C., & Drevets W. C. (2008). A neural model of voluntary and automatic emotion regulation: Implications for understanding the pathophysiology and neurodevelopment of bipolar disorder. Molecular Psychiatry, 13(9), 833-857. https://doi.org/10.1038/mp.2008.65 |
| [85] |
Pruessner L., Barnow S., Holt D. V., Joormann J., & Schulze K. (2020). A cognitive control framework for understanding emotion regulation flexibility. Emotion, 20(1), 21-29. https://doi.org/10.1037/emo0000658
doi: 10.1037/emo0000658 URL pmid: 31961173 |
| [86] | Qiu X., He Z., Cao X., & Zhang D. (2023). Transcranial magnetic stimulation and transcranial direct current stimulation affect explicit but not implicit emotion regulation: A meta-analysis. Behavioral and Brain Functions, 19(1), 15. https://doi.org/10.1186/s12993-023-00217-8 |
| [87] |
Quinn M. E., Stange J. P., Jenkins L. M., Corwin S., DelDonno S. R., Bessette K. L., Welsh R. C., & Langenecker S. A. (2018). Cognitive control and network disruption in remitted depression: A correlate of childhood adversity. Social Cognitive and Affective Neuroscience, 13(10), 1081-1090. https://doi.org/10.1093/scan/nsy077
doi: 10.1093/scan/nsy077 URL pmid: 30285231 |
| [88] |
Raij T., Nummenmaa A., Marin M. F., Porter D., Furtak S., Setsompop K., & Milad M. R. (2018). Prefrontal cortex stimulation enhances fear extinction memory in humans. Biological Psychiatry, 84(2), 129-137. https://doi.org/10.1016/j.biopsych.2017.10.022
doi: S0006-3223(17)32144-3 URL pmid: 29246436 |
| [89] | Rive M. M., Van Rooijen G., Veltman D. J., Phillips M. L., Schene A. H., & Ruhé H. G. (2013). Neural correlates of dysfunctional emotion regulation in major depressive disorder. A systematic review of neuroimaging studies. Neuroscience & Biobehavioral Reviews, 37(10), 2529-2553. https://doi.org/10.1016/j.neubiorev.2013.07.018 |
| [90] |
Rock P. L., Roiser J. P., Riedel W. J., & Blackwell A. D. (2014). Cognitive impairment in depression: A systematic review and meta-analysis. Psychological Medicine, 44(10), 2029-2040. https://doi.org/10.1017/S0033291713002535
doi: 10.1017/S0033291713002535 URL pmid: 24168753 |
| [91] |
Roy M., Shohamy D., & Wager T. D. (2012). Ventromedial prefrontal-subcortical systems and the generation of affective meaning. Trends in Cognitive Sciences, 16(3), 147-156. https://doi.org/10.1016/j.tics.2012.01.005
doi: 10.1016/j.tics.2012.01.005 URL pmid: 22310704 |
| [92] | Saturnino G. B., Madsen K. H., & Thielscher A. (2021). Optimizing the electric field strength in multiple targets for multichannel transcranial electric stimulation. Journal of Neural Engineering, 18(1), 014001. https://doi.org/10.1088/1741-2552/abca15 |
| [93] | Sergiou C. S., Santarnecchi E., Romanella S. M., Wieser M. J., Franken I. H. A., Rassin E. G. C., & van Dongen J. D. M. (2022). Transcranial direct current stimulation targeting the ventromedial prefrontal cortex reduces reactive aggression and modulates electrophysiological responses in a forensic population. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 7(1), 95-107. https://doi.org/10.1016/j.bpsc.2021.05.007 |
| [94] |
Silvers J. A., & Moreira J. F. G. (2019). Capacity and tendency: A neuroscientific framework for the study of emotion regulation. Neuroscience Letters, 693, 35-39. https://doi.org/10.1016/j.neulet.2017.09.017
doi: S0304-3940(17)30751-6 URL pmid: 28899785 |
| [95] |
Smith R., & Lane R. D. (2015). The neural basis of one’s own conscious and unconscious emotional states. Neuroscience and Biobehavioral Reviews, 57, 1-29. https://doi.org/10.1016/j.neubiorev.2015.08.003
doi: 10.1016/j.neubiorev.2015.08.003 URL pmid: 26363579 |
| [96] |
Snyder H. R. (2013). Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: A meta-analysis and review. Psychological Bulletin, 139(1), 81-132. https://doi.org/10.1037/a0028727
doi: 10.1037/a0028727 URL pmid: 22642228 |
| [97] |
Sotres-Bayon F., & Quirk G. J. (2010). Prefrontal control of fear: More than just extinction. Current Opinion in Neurobiology, 20(2), 231-235. https://doi.org/10.1016/j.conb.2010.02.005
doi: 10.1016/j.conb.2010.02.005 URL pmid: 20303254 |
| [98] | Sydnor V. J., Cieslak M., Duprat R., Deluisi J., Flounders M. W., Long H., … Oathes D. J. (2022). Cortical- subcortical structural connections support transcranial magnetic stimulation engagement of the amygdala. Science Advances, 8(25), 1-14. https://doi.org/10.1126/sciadv.abn5803 |
| [99] |
Tang Y., Mo L., Peng Z., Li Y., & Zhang D. (2025). Causal enhancement of cognitive reappraisal through synchronized dorsolateral and ventrolateral prefrontal cortex activity. Emotion. Advance online publication, 25(6), 1418-1428. https://doi.org/10.1037/emo0001507
doi: 10.1037/emo0001507 URL pmid: 39977692 |
| [100] |
Townsend J. D., Torrisi S. J., Lieberman M. D., Sugar C. A., Bookheimer S. Y., & Altshuler L. L. (2013). Frontal-amygdala connectivity alterations during emotion downregulation in bipolar I disorder. Biological Psychiatry, 73(2), 127-135. https://doi.org/10.1016/j.biopsych.2012.06.030
doi: 10.1016/j.biopsych.2012.06.030 URL pmid: 22858151 |
| [101] |
Troy A. S., Shallcross A. J., Brunner A., Friedman R., & Jones M. C. (2018). Cognitive reappraisal and acceptance: Effects on emotion, physiology, and perceived cognitive costs. Emotion, 18(1), 58-74. https://doi.org/10.1037/emo0000371
doi: 10.1037/emo0000371 URL pmid: 29154585 |
| [102] |
Urry H. L., van Reekum C. M., Johnstone T., & Davidson R. J. (2009). Individual differences in some (but not all) medial prefrontal regions reflect cognitive demand while regulating unpleasant emotion. NeuroImage, 47(3), 852-863. https://doi.org/10.1016/j.neuroimage.2009.05.069
doi: 10.1016/j.neuroimage.2009.05.069 URL pmid: 19486944 |
| [103] | Van't Wout M., Longo S. M., Reddy M. K., Philip N. S., Bowker M. T., & Greenberg B. D. (2017). Transcranial direct current stimulation may modulate extinction memory in posttraumatic stress disorder. Brain Behavior. 7(5), e00681. https://doi.org/10.1002/brb3.681 |
| [104] |
Van't Wout M., Mariano T. Y., Garnaat S. L., Reddy M. K., Rasmussen S. A., & Greenberg B. D. (2016). Can transcranial direct current stimulation augment extinction of conditioned fear? Brain Stimulation. 9(4), 529-536. https://doi.org/10.1016/j.brs.2016.03.004
doi: 10.1016/j.brs.2016.03.004 URL pmid: 27037186 |
| [105] | Velasco E. R., Florido A., Milad M. R., & Andero R. (2019). Sex differences in fear extinction. Neuroscience and Biobehavioral Reviews, 103 (11), 81-108. https://doi.org/10.1016/j.neubiorev.2019.05.020 |
| [106] | Vicario, C. M., Salehinejad M. A., Avenanti A., & Nitsche M. A. (2020). Transcranial direct current stimulation (tDCS) in anxiety disorders. In B.Dell’Osso & G. DiLorenzo (Eds.) Non invasive brain stimulation in psychiatry and clinical neurosciences (pp. 301-317). Springer. https://doi.org/10.1007/978-3-030-43356-7_21 |
| [107] | Vilgis V., Silk T. J., & Vance A. (2015). Executive function and attention in children and adolescents with depressive disorders: A systematic review. European Child & Adolescent Psychiatry, 24(4), 365-384. https://doi.org/10.1007/s00787-015-0675-7 |
| [108] | Wang H. Y., Xu G. Q., Ni M. F., Zhang C. H., Li X. L., Chang Y., Sun X. P., & Zhang B. W. (2021). Neural basis of implicit cognitive reappraisal in panic disorder: An event-related fMRI study. Journal of Translational Medicine, 19(1), 304. https://doi.org/10.1186/s12967-021-02968-2 |
| [109] | Wang H. Y., Xu G. Q., Ni M. F., Zhang C. H., Sun X. P., Chang Y., & Zhang B. W. (2017). Neural mechanisms of implicit cognitive reappraisal: Preceding descriptions alter emotional response to unpleasant images. Neuroscience, 347, 65-75. https://doi.org/10.1016/j.neuroscience.2017.01.047 |
| [110] | Wang H. Y., You H. L., Song C. L., Zhou L., Wang S. Y., Li X. L., Liang Z. H., & Zhang B. W. (2024). Shared and distinct prefrontal cortex alterations of implicit emotion regulation in depression and anxiety: An fNIRS investigation. Journal of Affective Disorders, 354, 126-135. https://doi.org/10.1016/j.jad.2024.03.032 |
| [111] |
Webb T. L., Miles E., & Sheeran P. (2012). Dealing with feeling: A meta-analysis of the effectiveness of strategies derived from the process model of emotion regulation. Psychological Bulletin, 138(4), 775-808. https://doi.org/10.1037/a0027600
doi: 10.1037/a0027600 URL pmid: 22582737 |
| [112] |
Wik G., Elbert T., Fredrikson M., Hoke M., & Ross B. (1997). Magnetic brain imaging of extinction processes in human classical conditioning. Neuroreport, 8(7), 1789-1792. https://doi.org/10.1097/00001756-199705060-00044
URL pmid: 9189934 |
| [113] |
Williams L. E., Bargh J. A., Nocera C. C., & Gray J. R. (2009). The unconscious regulation of emotion: Nonconscious reappraisal goals modulate emotional reactivity. Emotion, 9(6), 847-854. https://doi.org/10.1037/a0017745
doi: 10.1037/a0017745 URL pmid: 20001127 |
| [114] | Wyczesany M., Adamczyk A. K., Ligeza T. S., Bereś A., & Marchewka A. (2021). Implicit induction of emotional control—A comparative fMRI investigation of self-control and reappraisal goal pursuit. Emotion, 21(7), 1379-1391. https://doi.org/10.1037/emo0000852 |
| [115] | Xie Y., Hu Z., Ma W., Sang B., & Wang M. (2019). Different neural correlates of automatic emotion regulation at implicit and explicit perceptual level: A functional magnetic resonance imaging study. I-Perception, 10(1), 1-13. https://doi.org/10.1177/2041669519831028 |
| [116] |
Yang Q., Tang P., Gu R., Luo W., & Luo Y. (2015). Implicit emotion regulation affects outcome evaluation. Social Cognitive and Affective Neuroscience, 10(6), 824-831. https://doi.org/10.1093/scan/nsu124
doi: 10.1093/scan/nsu124 URL pmid: 25332404 |
| [117] | Yuan J., Long Q., Li X., Deng Z., Ma B., Chen S., & Yang J. (2019). Regulatory effect of implicit acceptance during outcome evaluation: The temporal dynamics in an event-related potential study. International Journal of Psychophysiology, 141(5), 37-44. https://doi.org/10.1016/j.ijpsycho.2019.05.003 |
| [118] |
Yuan J., Zhang Y., Zhao Y., Gao K., Tan S., & Zhang D. (2022). The Emotion-regulation benefits of implicit reappraisal in clinical depression: Behavioral and electrophysiological evidence. Neuroscience Bulletin, 39, 973-983. https://doi.org/10.1007/s12264-022-00973-z
doi: 10.1007/s12264-022-00973-z URL pmid: 36355339 |
| [119] | Zabik N. L., Peters C., Iadipaolo A., Marusak H. A., & Rabinak C. A. (2023). Comparison of behavioral and brain indices of fear renewal during a standard vs. novel immersive reality pavlovian fear extinction paradigm in healthy adults. Behavioural Brain Research, 437, 114154. https://doi.org/10.1016/j.bbr.2022.114154 |
| [120] |
Zhang Q., Chen T., Liu S., Liu X., Zhang Y., Yu F., … Zhu C. (2023). Effects of high-definition transcranial direct current stimulation on implicit emotion regulation of social pain in healthy individuals. Journal of Affective Disorders, 338, 74-82. https://doi.org/10.1016/j.jad.2023.05.075
doi: 10.1016/j.jad.2023.05.075 URL pmid: 37269884 |
| [121] | Zhang Y., Chen S., Deng Z., Yang J., & Yuan J. (2020). Benefits of implicit regulation of instructed fear: Evidence from neuroimaging and functional connectivity. Frontiers in Neuroscience, 14(4), 1-13. https://doi.org/10.3389/fnins.2020.00201 |
| [122] | Zhang Y., Li S., Gao K., Li Y., Yuan J., & Zhang D. (2023). Implicit, but not explicit, emotion regulation relieves unpleasant neural responses evoked by high- intensity negative images. Neuroscience Bulletin, 39(8), 1278-1288. https://doi.org/10.1007/s12264-023-01036-7 |
| [123] | Zhang Y., Shi W., Wang H., Liu M., & Tang D. (2021). The impact of acute exercise on implicit cognitive reappraisal in association with left dorsolateral prefronta activation: A fNIRS study. Behavioural Brain Research, 406(2), 113233. https://doi.org/10.1016/j.bbr.2021.113233 |
| [124] | Zhu C., Li P., Li Y., Jiang Y., Liu D., & Luo W. (2022). Implicit emotion regulation improves arithmetic performance: An ERP study. Cognitive, Affective and Behavioral Neuroscience, 22(3), 574-585. https://doi.org/10.3758/s13415-021-00979-6 |
| [125] |
Zilverstand A., Parvaz M. A., & Goldstein R. Z. (2017). Neuroimaging cognitive reappraisal in clinical populations to define neural targets for enhancing emotion regulation. A systematic review. NeuroImage, 151, 105-116. https://doi.org/10.1016/j.neuroimage.2016.06.009
doi: S1053-8119(16)30227-0 URL pmid: 27288319 |
| [1] | 谢宇, 郑弘欣, 刘怡资, 禹红刚, 杨成赫. 大模型在抑郁症筛查与诊断中的应用[J]. 心理科学进展, 2026, 34(3): 424-440. |
| [2] | 田柳青, 陈彦霖, 林美玲, 陈栋, 王亮. 侵入式脑机接口应用:记忆的解码与调控[J]. 心理科学进展, 2026, 34(2): 191-209. |
| [3] | 董耀华, 汤煜尧, 张丹丹. 经颅交流电刺激在心理学研究中的应用[J]. 心理科学进展, 2026, 34(2): 239-250. |
| [4] | 彭玉佳, 王愉茜, 鞠芊芊, 刘峰, 徐佳. 贝叶斯框架下社交焦虑的社会认知特性[J]. 心理科学进展, 2025, 33(8): 1267-1274. |
| [5] | 楚克群, 朱风书. 运动干预对攻击行为的抑制及其作用机制[J]. 心理科学进展, 2025, 33(7): 1257-1266. |
| [6] | 刘永进, 杨雪, 杜欣欣, 嵇文麒, 臧寅垠, 官锐园, 宋森, 钱铭怡, 牟文婷. 融合机器学习技术的阈下抑郁神经生理机制及干预[J]. 心理科学进展, 2025, 33(6): 887-904. |
| [7] | 夏熠, 张婕, 张火垠, 雷怡, 窦皓然. 焦虑个体趋避冲突失调的认知神经机制[J]. 心理科学进展, 2025, 33(3): 477-493. |
| [8] | 高伟, 李艳萍, 黄悦媛, 袁加锦. 目标与情境转换对情绪调节灵活性的作用机制[J]. 心理科学进展, 2025, 33(2): 202-211. |
| [9] | 唐苏勤, 彭闻捷, 余茵琪, 符仲芳. 丧亲人群网络化心理干预效果的系统综述与元分析[J]. 心理科学进展, 2025, 33(2): 256-273. |
| [10] | 苑墨桐, 蔡雨霏, 孙宏伟, 李妍妍, 王亮. 幻觉的神经和计算机制[J]. 心理科学进展, 2025, 33(12): 2156-2167. |
| [11] | 靳帅, 刘思佳, 李爽, 刘志远, 郭秀艳. 后悔情绪及其调节[J]. 心理科学进展, 2025, 33(12): 2182-2195. |
| [12] | 赵立, 白莎. 数媒时代焦虑、抑郁与社会比较的关系[J]. 心理科学进展, 2025, 33(1): 92-106. |
| [13] | 温秀娟, 马毓璟, 谭斯祺, 李芸, 刘文华. 身体还是认知努力的损害?抑郁症努力奖赏动机评估及计算模型应用[J]. 心理科学进展, 2025, 33(1): 107-122. |
| [14] | 雷怡, 梅颖, 王金霞, 袁子昕. 焦虑青少年无意识恐惧的神经机制及干预[J]. 心理科学进展, 2024, 32(8): 1221-1232. |
| [15] | 丁颖, 汪紫滢, 李卫东. 抑郁症疼痛加工的行为特点及神经机制[J]. 心理科学进展, 2024, 32(8): 1315-1327. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||